Metabolic Syndrome in Children
- An epidemic of childhood obesity (often denied by the parents) has resulted in a dramatic rise in metabolic syndrome (MS) and diabetes, both precursors to heart disease. Pediatric MS is a strong predictor of adulthood MS, subclinical atherosclerosis (silent heart disease), and diabetes.1
- The prevalence of MS in children varies widely from 4% overall to as high as 30% in overweight US children.2, 3 Approximately one-third of obese children and one-half of severely obese children in the US have MS and are likely to become diabetic before 30 years of age.4, 5
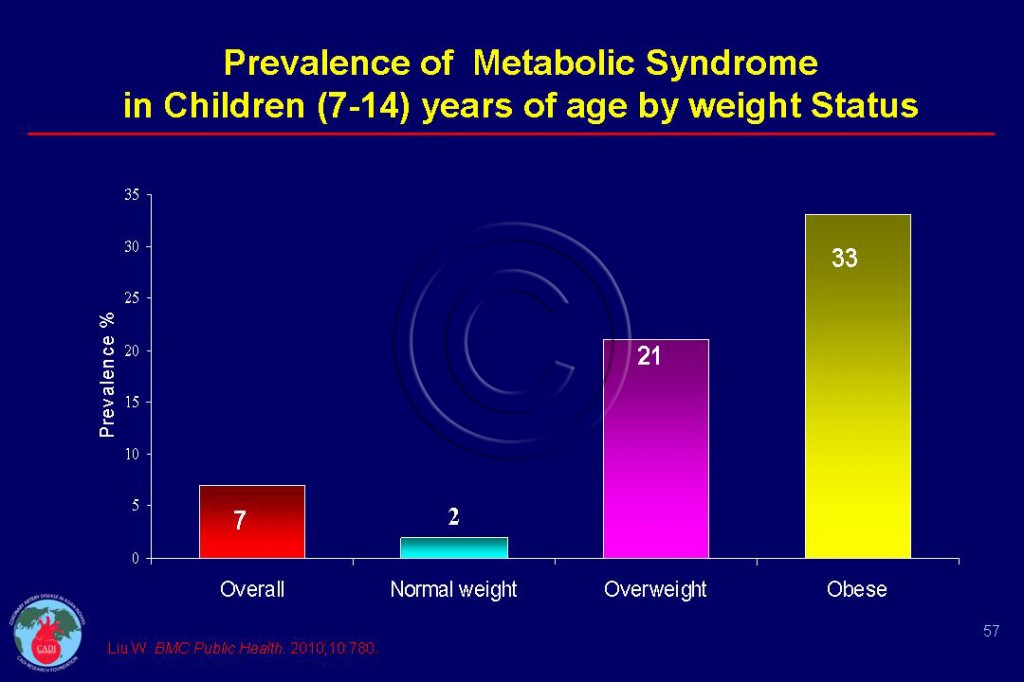
- China is fast approaching the US with regard to pediatric obesity and MS with 10% of Chinese children being overweight and almost 7% obese. The prevalence of MS increases from 2% in normal weight children to 21% in overweight and 33% among obese children (Figure 057).6
- Obesity, especially abdominal obesity, and insulin resistance are directly related to the development of the MS and CVD risk in children and youth.7 MS and insulin resistance are closely related that the former may be an expression of the latter.
- Prediabetes and nonalcoholic fatty liver disease (NAFLD) are more common in children and adolescents with MS. Therefore children with MS should be evaluated for these 2 conditions.8
- Larger than average offspring of diabetic mothers as well as children exposed to maternal obesity are at significant risk of developing MS in childhood. Conversely higher offspring birth weight predicts the metabolic syndrome in mothers but not fathers.9 Given the increased obesity prevalence, these findings have implications for perpetuating the cycle of obesity, insulin resistance, and their consequences in subsequent generations.10
- Waist circumference (WC) in children (a surrogate for visceral adiposity) is a stronger predictor of onset of the MS in adulthood than all other measures of adiposity.7 Children initially in the top 25% for WC had at least five times the risk of MS as young adults compared to those in bottom 25%. 11
- Even if the child had a pretty low WC in childhood, a huge increase in WC is going to increase the risk of MS substantially. Each 10-cm increment in childhood WC was associated with a doubling of the risk of MS in adulthood.11, 12
- The dramatic increase in prevalence of childhood obesity, especially the WC, throughout the world could result in a dangerous increase in MS, diabetes, and CVD occurring in early adulthood.11, 12 When diabetes begins in childhood, the risk for accelerated atherosclerosis is increased beyond that seen in those who develop this diagnosis as adults. 13
Diagnosis of Metabolic Syndrome in Children
- MS in adults is defined as the clustering of interrelated cardiovascular risk factors including obesity, insulin resistance, inflammation and others. In children and adolescents, there is no universally accepted definition of the MS, although several definitions have been proposed, using criteria adapted from adult standards using gender and age-dependent normal values. The International Diabetes Federation (IDF) criteria for defining MS in children is given below.14
|
The IDF criteria for MS in children |
|
| 6-9 years | Obesity (defined as >90th percentile of WC, followed by further measurements as indicated by family history |
| 10-15 years | Obesity (defined as WC>90th percentile), followed by the adult criteria for triglycerides, HDL-C, blood pressure, and glucose. |
| > 16 years | Same criteria as adults |
| WC= waist circumference | |
- Obesity, weight gain and poor fitness are important risk factors for MS.15 Comprehensive behavioral modification in overweight children reduces body weight, improves body composition, and positively modifies many of the components of the MS within 3 months, and these effects are maintained if the behavior modification is continued.16 17 18In fact, there is no specific treatment for MS in children, other than reducing obesity, increasing physical activity, and treating the various components of the MS (hypertension or hyperlipidemia).
- There is growing evidence that efforts to prevent weight gain must begin in early life. Furthermore, low-birth weight followed by rapid excess weight gain in childhood and adolescence increase the risk of developing MS, diabetes and CVD.19 In small studies, metformin has been used effectively in adolescents with diabetes to decrease BMI and improve glucose tolerance.20, 21
Sources
1. Magnussen CG, Koskinen J, Chen W, et al. Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa Heart Study and the Cardiovascular Risk in Young Finns Study. Circulation. Oct 19 2010;122(16):1604-1611.
2. Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. Aug 2003;157(8):821-827.
3. Duncan GE, Li SM, Zhou XH. Prevalence and trends of a metabolic syndrome phenotype among u.s. Adolescents, 1999-2000. Diabetes Care. Oct 2004;27(10):2438-2443.
4. Enas EA. How to Beat the Heart Disease Epidemic among South Asians: A Prevention and Management Guide for Asian Indians and their Doctors. Downers Grove: Advanced Heart Lipid Clinic USA; 2010.
5. Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003-2006. Natl Health Stat Report. May 5 2009(13):1-7.
6. Liu W., Lin R, Liu A, Du L, Chen Q. Prevalence and association between obesity and metabolic syndrome among Chinese elementary school children: a school-based survey. BMC Public Health. 2010;10:780.
7. Schmidt MD, Dwyer T, Magnussen CG, Venn AJ. Predictive associations between alternative measures of childhood adiposity and adult cardio-metabolic health. International journal of obesity (2005). Sep 28 2010.
8. Love-Osborne KA, Nadeau KJ, Sheeder J, Fenton LZ, Zeitler P. Presence of the metabolic syndrome in obese adolescents predicts impaired glucose tolerance and nonalcoholic fatty liver disease. J Adolesc Health. Jun 2008;42(6):543-548.
9. Yajnik CS, Joglekar CV, Pandit AN, et al. Higher offspring birth weight predicts the metabolic syndrome in mothers but not fathers 8 years after delivery: the Pune Children’s Study. Diabetes. Aug 2003;52(8):2090-2096.
10. Boney CM, Verma A, Tucker R, Vohr BR. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics. Mar 2005;115(3):e290-296.
11. Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. Feb 11 2010;362(6):485-493.
12. Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and international association for the Study of Obesity. Circulation. Oct 20 2009;120(16):1640-1645.
13. Crespo CJ, Smit E, Troiano RP, Bartlett SJ, Macera CA, Andersen RE. Television watching, energy intake, and obesity in US children: results from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. Mar 2001;155(3):360-365.
14. Steinberger J, Daniels SR, Eckel RH, et al. Progress and challenges in metabolic syndrome in children and adolescents: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular Nursing; and Council on Nutrition, Physical Activity, and Metabolism. Circulation. Feb 3 2009;119(4):628-647.
15. Carnethon MR, Gidding SS, Nehgme R, Sidney S, Jacobs DR, Jr., Liu K. Cardiorespiratory fitness in young adulthood and the development of cardiovascular disease risk factors. Jama. Dec 17 2003;290(23):3092-3100.
16. Nemet D, Barkan S, Epstein Y, Friedland O, Kowen G, Eliakim A. Short- and long-term beneficial effects of a combined dietary-behavioral-physical activity intervention for the treatment of childhood obesity. Pediatrics. Apr 2005;115(4):e443-449.
17. Woo KS, Chook P, Yu CW, et al. Effects of diet and exercise on obesity-related vascular dysfunction in children. Circulation. Apr 27 2004;109(16):1981-1986.
18. Carnethon MR, Loria CM, Hill JO, Sidney S, Savage PJ, Liu K. Risk factors for the metabolic syndrome: the Coronary Artery Risk Development in Young Adults (CARDIA) study, 1985-2001. Diabetes Care. Nov 2004;27(11):2707-2715.
19. Enas EA, Mohan V, Deepa M, Farooq S, Pazhoor S, Chennikkara H. The metabolic syndrome and dyslipidemia among Asian Indians: a population with high rates of diabetes and premature coronary artery disease. Journal of the cardiometabolic syndrome. Fall 2007;2(4):267-275.
20. Jones KL, Arslanian S, Peterokova VA, Park JS, Tomlinson MJ. Effect of metformin in pediatric patients with type 2 diabetes: a randomized controlled trial. Diabetes Care. Jan 2002;25(1):89-94.
21.Freemark M, Bursey D. The effects of metformin on body mass index and glucose tolerance in obese adolescents with fasting hyperinsulinemia and a family history of type 2 diabetes. Pediatrics. Apr 2001;107(4):E55.