South Asian Modified NCEP Criteria for Metabolic Syndrome
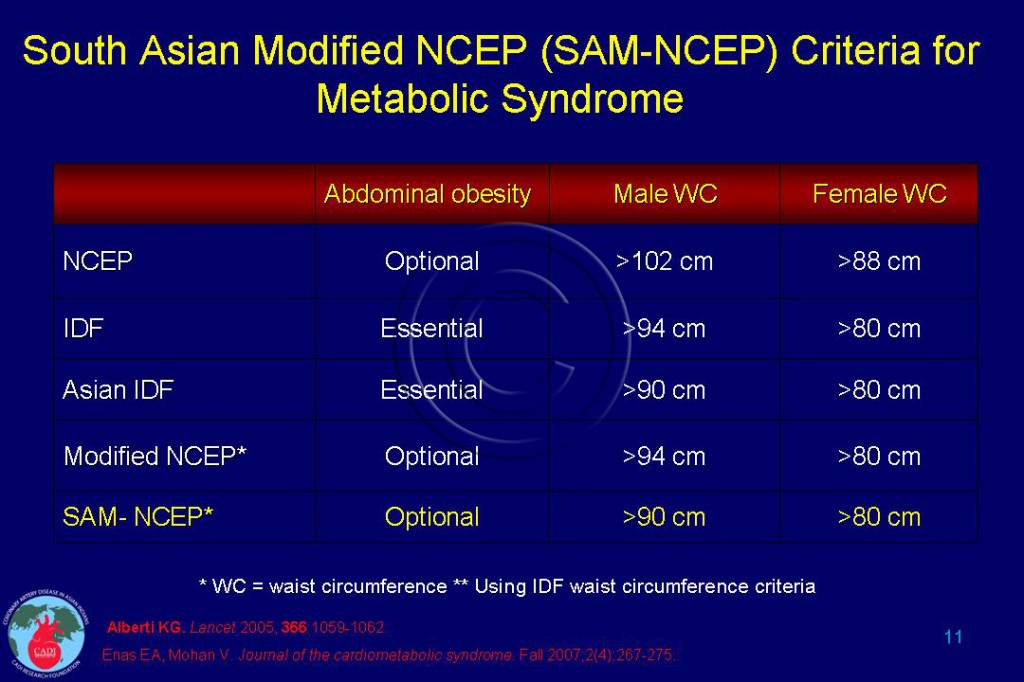
- Although National Cholesterol Education Program (NCEP) does not provide ethnic-specific cutoff points for waist circumference (WC), the 2005 American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement on MS endorses the lower WC for all Asian Americans (<90 cm for men and <80 cm for women).1
- In 2007, Enas and Mohan have proposed for the first time, the South Asian Modified (SAM)-NCEP Criteria which follows the NCEP criteria for metabolic syndrome (MS) except for the inclusion of South Asian-specific WC cutoff points for abdominal obesity as recommended by the International Diabetic Federation (IDF).2, 3,4 Thus, unlike the IDF criteria, abdominal obesity is considered optional, not essential in SAM-NCEP criteria Table 011.2
- Lee and associates5 studied the prevalence of MS in the presence and absence of abdominal obesity in a multiethnic Asian population in Singapore. From the population-based cohort study (baseline 1992-1995), 4,334 healthy individuals were grouped by the presence or absence of MS and abdominal obesity and followed up for an average of 9.6 years. The prevalence of MS was 18% by IDF criteria but increased to 26% by the SAM-NCEP criteria. This means that 8% of the participants had 3 or more MS components in the absence of abdominal obesity.
- Thus, making abdominal obesity as an essential rather than an optional component to diagnose MS would fail to identify a fairly large proportion of individuals with MS (44%). Specifically, prevalence of MS among Asian Indians would increase by 50%. With application of the SAM-NCEP criteria, Asian Indians had higher rates of MS (38%) than Chinese (24%) and Malays (30%).4,5
- The results of this pioneering study also showed that having MS either with or without abdominal obesity conferred similar CAD risk. There were 135 first-time CAD events during nearly 10 years of follow up. Cox’s proportional hazards model was used to obtain adjusted hazard ratios (HRs) for risk of a first-time CAD event.
- Compared with individuals without MS, the risk of first CAD event was nearly identical in people with and without abdominal obesity. The risk of CAD was 2.8for those with MS with abdominal obesity and 2.5 for those with MS and no abdominal obesity.4,5
- This study has clearly demonstrated that designating abdominal obesity as an optional rather than essential criterion identifies more individuals at risk of CAD. Conversely, this study suggests that including abdominal obesity as an essential component for the diagnosis of MS as proposed by IDF, fails to identify approximately 50% of those who are at high risk of CAD. A similar 50% increase in MS is noted in other Asian populations when SAM-NCEP criteria are used (19% IDF vs. 29% SAM-NCEP) without any decrease in the odds ratio for CAD.6
Prevalence of MS among Asian Indians using SAM-NCEP criteria
- Among South Asians, the prevalence of MS is higher by 30% to 50% when SAM-NCEP criteria are applied compared with NCEP criteria and 20% higher compared with IDF criteria.
- The prevalence of MS for Asian Indians in Singapore increased from 27% with NCEP criteria to 35% with SAM-NCEP criteria.7
- In CURES, the prevalence of MS increased from 18% with NCEP criteria to 30% with SAM–NCEP criteria, whereas another study from the same city (Chennai) reported MS prevalence of 41% with criteria very similar to those of SAM-NCEP.8
- A recent study from rural Andhra Pradesh, India, involving 4,535 adults aged 30 years and older showed a prevalence of MS by NCEP criteria of 27% in men and 18% in women, which increased to 33% and 24%, respectively, when SAM-NCEP criteria were applied. 9
- In a large, contemporary, multicenter study involving 19,973 subjects in India, the prevalence of MS was 27% with NCEP criteria but increased to 35% with SAM-NCEP criteria.10 In addition, there was wide regional variation in the prevalence of MS from as low as 13% to as high as 47% .10
- This increase in prevalence of MS in South Asians is in sharp contrast to that of the US population. If abdominal obesity were not a prerequisite, the prevalence of MS with IDF criteria would increase only slightly from 39% to 40%.11
- The overall prevalence of abdominal obesity is around 50% among Asian Indians when the IDF WC cutoff point is used, and 10% to 20% when the NCEP WC cutoff point is applied.2 This explains why SAM-NCEP is better suited for South Asians.
- The overall prevalence of MS identified with SAM-NCEP criteria among Asian Indians is 30% to 40%, which is double that of Europeans (prevalence is 15%-20%) and similar to that of Americans (prevalence is 35%-40%).2, 8, 12-14
- The controversy about the definition of MS has been finally resolved and there is now a single global definition with specific lower cutpoints for waist circumference for Asian Indians and other Asians as was originally proposed by Enas and Mohan.15, 16
Sources
1. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. Oct 25 2005;112(17):2735-2752.
2. Enas EA, Mohan V, Deepa M, Farooq S, Pazhoor S, Chennikkara H. The metabolic syndrome and dyslipidemia among Asian Indians: a population with high rates of diabetes and premature coronary artery disease. Journal of the cardiometabolic syndrome. Fall 2007;2(4):267-275.
3. Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: an american heart association/national heart, lung, and blood institute scientific statement: executive summary. Circulation. Oct 25 2005;112(17):e285-290.
4. Grundy SM. Metabolic syndrome: connecting and reconciling cardiovascular and diabetes worlds. J Am Coll Cardiol. Mar 21 2006;47(6):1093-1100.
5. Lee J, Ma S, Heng D, et al. Should central obesity be an optional or essential component of the metabolic syndrome? Ischemic heart disease risk in the Singapore Cardiovascular Cohort Study. Diabetes Care. Feb 2007;30(2):343-347.
6. Moon JY, Park S, Rhee JH, et al. The applicability of the Asian modified criteria of the metabolic syndrome in the Korean population. Int J Cardiol. Jan 2 2007;114(1):83-89.
7. Tan CE, Ma S, Wai D, Chew SK, Tai ES. Can we apply the National Cholesterol Education Program Adult Treatment Panel definition of the metabolic syndrome to Asians? Diabetes Care. May 2004;27(5):1182-1186.
8. Ramachandran A, Snehalatha C, Satyavani K, Sivasankari S, Vijay V. Metabolic syndrome in urban Asian Indian adults–a population study using modified ATP III criteria. Diabetes Res Clin Pract. Jun 2003;60(3):199-204.
9. Chow CK, Naidu S, Raju K, et al. Significant lipid, adiposity and metabolic abnormalities amongst 4535 Indians from a developing region of rural Andhra Pradesh. Atherosclerosis. Apr 26 2007.
10. Reddy KS, Prabhakaran D, Chaturvedi V, et al. Methods for establishing a surveillance system for cardiovascular diseases in Indian industrial populations. Bull World Health Organ. Jun 2006;84(6):461-469.
11. Cheung BM, Ong KL, Man YB, Wong LY, Lau CP, Lam KS. Prevalence of the metabolic syndrome in the United States National Health and Nutrition Examination Survey 1999-2002 according to different defining criteria. Journal of clinical hypertension (Greenwich, Conn. Aug 2006;8(8):562-570.
12. Tillin T, Forouhi N, Johnston DG, McKeigue PM, Chaturvedi N, Godsland IF. Metabolic syndrome and coronary heart disease in South Asians, African-Caribbeans and white Europeans: a UK population-based cross-sectional study. Diabetologia. Apr 2005;48(4):649-656.
13. Chambers J. The age and gender relted prevalence of the metabolic syndrome among UK Indian Asians and European whites:First results from the LondonLife Sciences Population (LOLIPOP) Study. Heart (British Cardiac Society). 2006;92(suppl):A11 (abstract).
14. Hu G, Qiao Q, Tuomilehto J, Balkau B, Borch-Johnsen K, Pyorala K. Prevalence of the metabolic syndrome and its relation to all-cause and cardiovascular mortality in nondiabetic European men and women. Arch Intern Med. May 24 2004;164(10):1066-1076.
15. Misra A, Khurana L. The metabolic syndrome in South Asians: epidemiology, determinants, and prevention. Metab Syndr Relat Disord. Dec 2009;7(6):497-514.
16. Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and international association for the Study of Obesity. Circulation. Oct 20 2009;120(16):1640-1645.