Primordial Prevention and Population based Strategies
- Primordial prevention is the prevention of the development of risk factors in the first place with lifestyle only and thus avoiding the use of medications to treat risk factors and expensive coronary procedures like coronary angioplasty and bypass surgery, saving money for the individual, family, and the society.
- It aims to prevent the occurrence of the risk factors themselves by optimizing lifestyles that are associated with low blood pressure and cholesterol, ideal body weight, and nonsmoking.1 Such strategy requires tackling the roots of CVD (cardiovascular disease) risk factors by health promotion, healthy public policies, and improved physical environments conducive to healthy lifestyles throughout the whole course of life, from conception to older age.2
- Such a strategy has been found to be highly effective in lowering the saturated fat intake and cholesterol level throughout the first 14 years of life. 3
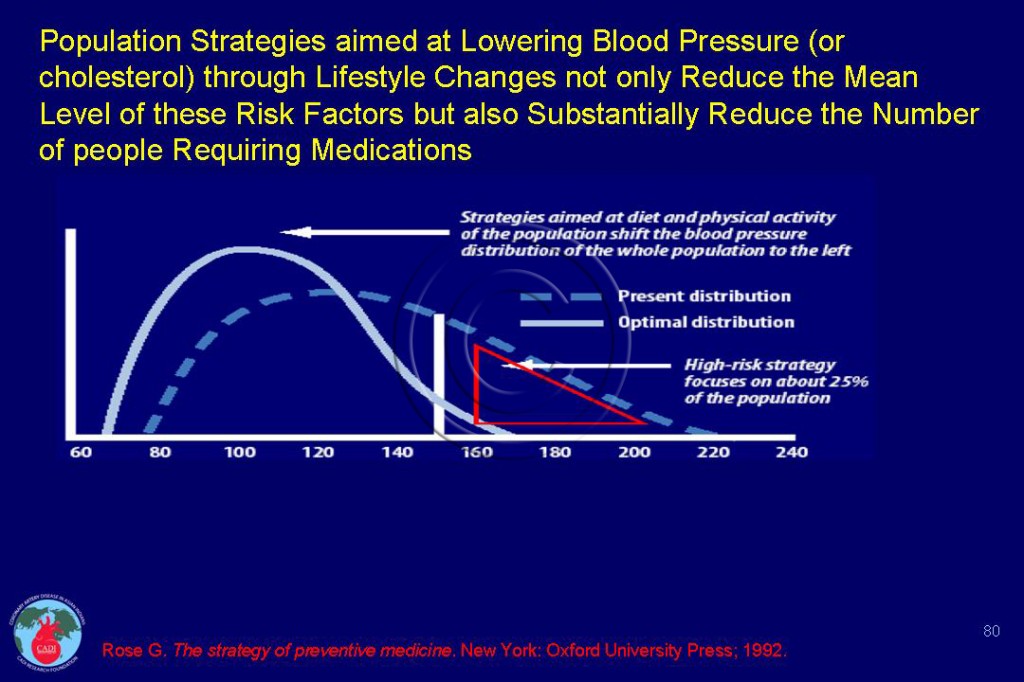
- The impact of population strategies to reduce the mean level of blood pressure and reduce the proportion of people requiring hypertension is given in Figure 080. The same can be achieved for cholesterol.
- More recent reports have proposed new affordable public health and healthcare recommendations with a high potential for impact.4-6 These include: 1) health information and communication strategies that improve population awareness about the benefits of healthy eating and physical activity; 2) fiscal measures that increase the price of unhealthy food content or reduce the cost of healthy foods rich in fiber; 3) regulatory measures that improve nutritional information or restrict the marketing of unhealthy foods to children.4
- Application of primordial prevention for the total population is called population-based strategy of prevention. The population-based strategy aims to lower the risk factors in the entire population through modification of lifestyle in the entire population or the country and have been successfully implemented in Finland, Mauritius, Norway and Poland.
- Three major life style changes; smoking cessation, healthy diet and increased physical activity will make a big difference in reducing the health care burden of these chronic disease. Very substantial health gains can be made for relatively modest expenditures on interventions. The 3 key specific population-wide lifestyle changes that have the maximum impact on changing population distributions of the risk factors are:
- Decrease in dietary saturated fat to lower blood cholesterol levels
- Decrease in salt intake to lower the blood pressure levels.
- Higher taxes, total advertisement bans and smoke free policies for tobacco control.
- The experiences in the US and Finland have clearly demonstrated that lowering the mean population serum cholesterol level has far greater impact than treatment of all those with high levels of cholesterol.7
- The population-strategy requires promoting a healthier life-style in the population as a whole by encouraging people to seek alternatives and making them available8. Implementation of many evidence-based interventions exists, but requires a sustained policy framework and strengthened institutional support.
- While much is known about the elements required for effective and safe prevention, little is known about how to deliver these reliably and affordably in new disease epicenters such as India (see Prevention in Asian Indians). If this could be achieved on a large scale throughout India, several million people would be saved each year from death or disability during the most economically productive years of their lives.
Advantages and Disadvantages of Population-based Strategies
- The population-based strategy can create a new generation in which low-risk is the rule and high-risk the exception. Most importantly, this ensures that children adopt healthy eating habits, slowing the rise in their cholesterol level with age, thereby creating a new generation with lower risk factor levels. In the US, UK, and many other countries, the change in cholesterol was mostly due to dietary changes not statin therapy.
- On the other hand, it requires promoting a healthier life-style in the population as a whole by encouraging people to seek alternatives and making them available.8 Implementation of many evidence-based interventions exists but requires a sustained policy framework and strengthened institutional support.
- Compliance with preventive measures is achievable only if the message is given repeatedly, consistently and unambiguously irrespective of the economic impact.8 It rests mainly on public education, media, legislation and government policy.9
- Strategies will have to be tailored to suit individual countries and the economies. This will require further concentrated effort, guided by a health strategy and involve effective partnerships among government, nongovernmental organizations, and the civil society more generally. This type of strategy is mostly achieved by establishing ad hoc policies and community interventions.
- It requires greater investment and planning for the implementation of life-style intervention. It is very dependent on the governments’ commitment and determination.9
- In summary, identification of and intervention on high risk individuals (“high risk strategy”) is helpful and cost effective concerning these individuals, but general risk factor changes in the population (“population-strategy”) is overwhelmingly most effective and cost-effective in reducing the disease rates in the population.
Sources
1. Labarthe DR. Prevention of cardiovascular risk factors in the first place. Prev Med. Dec 1999;29(6 Pt 2):S72-78.
2.Paradis G, Chiolero A. The cardiovascular and chronic diseases epidemic in low- and middle-income countries a global health challenge. J Am Coll Cardiol. Apr 26 2011;57(17):1775-1777.
3. Niinikoski H, Lagstrom H, Jokinen E, et al. Impact of repeated dietary counseling between infancy and 14 years of age on dietary intakes and serum lipids and lipoproteins: the STRIP study. Circulation. Aug 28 2007;116(9):1032-1040.
4. Cecchini M, Sassi F, Lauer JA, Lee YY, Guajardo-Barron V, Chisholm D. Tackling of unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness. Lancet. Nov 20 2010;376(9754):1775-1784.
5. Samb B, Desai N, Nishtar S, et al. Prevention and management of chronic disease: a litmus test for health-systems strengthening in low-income and middle-income countries. Lancet. Nov 20 2010;376(9754):1785-1797.
6. Lock K, Smith RD, Dangour AD, et al. Health, agricultural, and economic eff ects of adoption of healthy diet recommendations. Lancet. Nov 13 2010;376(9753):1699-1709.
7. Enas EA, Jacob S. Decline of CAD in developed countries: Lessons for India. In: Sethi K, ed. Coronary Artery Disease in Indians – A Global Perspective. Mumbai: Cardiological Society of India; 1998:98 -113.
8. Pais PS. Early intervention and prevention of myocardial infarction. J Hypertens Suppl. Apr 2006;24(2):S25-30.
9. Enas EA, Yusuf S, Sharma S. Coronary artery disease in South Asians; second meeting of the International Working Group, 16 March 1997, Anaheim, California. Indian heart journal. 1998;50:105-113.