Secondary prevention
- Individuals with documented coronary artery disease (CAD) have 5 to 7 timesthe risk ofhaving a heart attack or dying compared to the general population.1 Secondary prevention refers to the preventive measures undertaken in people with known CAD to prevent a second heart attack, heart failure, sudden death, as well as coronary angioplasty, stents, bypass surgery. It has the most rapid initial impact on recurrent cardiovascular disease (CVD) which is far more common in this population.2, 3
- Although secondary prevention reduces the rates of recurrent heart attacks, it does nothing to prevent the larger burden of first attacks. It is worth highlighting a heart attack or sudden death is the first manifestation of CAD in half of all women and two-thirds of all men. It ignores the long-term cost-effective goal of preventing future high risk of CVD among the youth. Of course, this strategy will do little to reduce the long-term burden of chronic disease (see Primary Prevention).
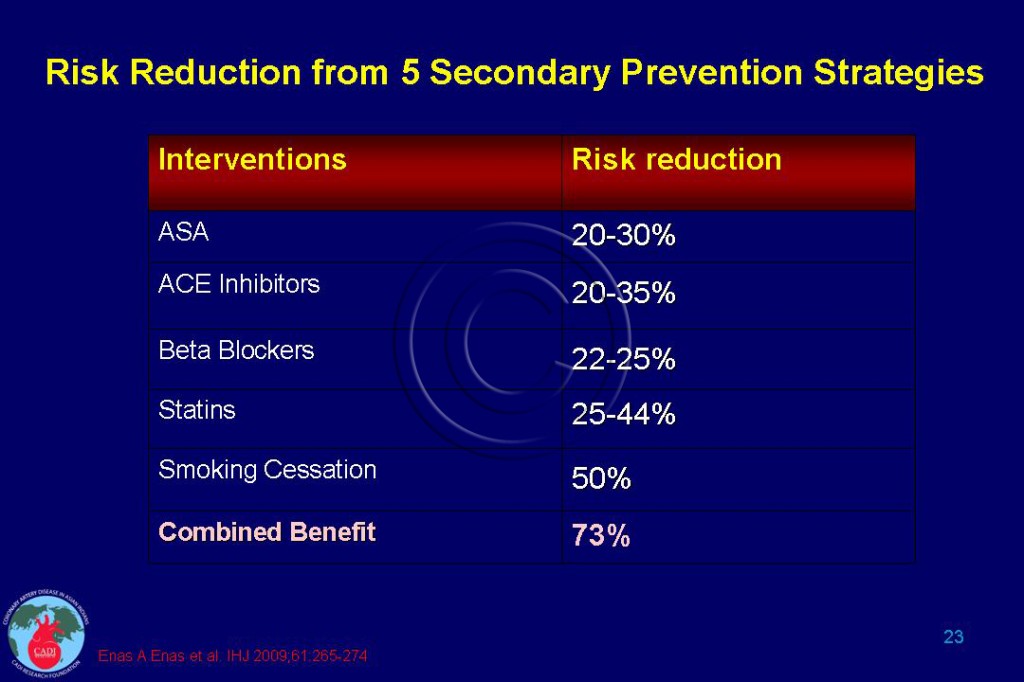
- The extent of benefit that can be achieved with various secondary prevention strategies are given in Table 023.
- Smoking cessation along with four life-saving medications can reduce the risk of a heart attack by 73% and the price of these medications have come done drastically yet the percentage of people with heart disease who are actually prescribed and taking these medications is 60-70% in the US.4
- A recent study from Rajasthan has documented suboptimal prescription of evidence-based medication for people with CAD. The prescription of the 4-drug combination of aspirin, β-blockers, angiotensin-converting enzyme inhibitors, and statins by physicians at all three levels of health care ranged from 43% in tertiary care to 28% in secondary care and only 7% in primary care facilities.5 The underuse of life saving medications is rampant in India and contributes to unnecessary death and disability (see CAD India).
The COURAGE Trial
- The overwhelming benefit of the use of guideline recommended medications was clearly demonstrated in the COURAGE trial in which optimal lifestyle modification and medical therapy was provided to all the participants with CAD. In this secondary prevention trial there was a very high use of evidence-based medicines; aspirin 96%, lipid-lowering therapy 97%, beta-blockers 85%, and 80% received all 3 medications.6
- A striking finding in this trial was absence of any additional benefit among those who received angioplasty or stent compared to those who received optimal medical management alone. Among patients with stable angina, all patients had marked improvements in health status during follow-up. The coronary angioplasty stent group had small, but significant, incremental benefits that disappeared by 36 months.7
- This trial shows that coronary angioplasty/stent and bypass surgery does not provide significant additional long term benefit over and beyond that achieved with optimal lifestyle modifications and the use of recommended medications. Cardiologists throughout the world must display enough courage to implement the message of COURAGE Trial.
Secondary Prevention around the World ─Lessons from PURE Study
- Effective preventive drugs for CAD and stroke are underused globally, with striking variation between countries at different stages of economic development. Even the use of accessible and inexpensive treatments such as aspirin (the most commonly used antiplatelet drug) varied seven-fold between low-income and high-income countries but the use of statins varied 20-fold.8
- In the Prospective Urban Rural Epidemiological (PURE) study, Yusuf and associates, recruited 153,996 adults (aged 35–70 years from 628 urban and rural communities) in 17 countries at various stages of economic development between January, 2003, and December, 2009. Of these countries, three were classified as high income, seven were upper-middle, three were lower-middle, and four were low-income by the World Bank definition. 5650 participants had a self-reported CAD event (median 5 years previously) and 2292 had stroke (4 years previously).8
|
Table 127A. The Differences in Use of Life-Saving Medications by Country Income Status |
||||
| Medications |
High |
Upper middle |
Lower middle |
Low |
| Antiplatelet drugs |
62% |
20-30% |
20% |
9% |
| Beta blockers |
40% |
25-36% |
9-13 |
10% |
| ACE inhibitors or ARBs |
50% |
24-36% |
10-11% |
5% |
| Statins |
66% |
16-25% |
5-6% |
3% |
| The proportion of those receiving none of the 4 essential drugs was |
13% |
48% |
68% |
83% |
| The proportion of participants taking three or more drugs |
44% |
13% |
3% |
3% |
- Overall, few individuals with CVD took antiplatelet drugs (25%), beta blockers (17%), ACE inhibitors or ARBs (20%), or statins (15%). The use of all 4 medications was highest in the high-income (44%) and lowest in low-income (3%) countries. The differences in use of these agents by country incomes are given in Table 127A.8
- Among participants who had CAD or stroke, 59% individuals were not taking any of the four proven effective drugs and only 3% were taking all four drug types. The proportion of those receiving no drug was lowest in high-income countries (13%), compared with 48% in upper middle-income countries, 68% in lower middle income countries, and 83% in low-income countries.8
- The highest proportion of participants taking three or more drugs lived in high-income countries (44%), compared with 13% in upper middle-income countries, 3% in lower middle-income countries, and low-income countries. 8
- Drug use was higher in urban than rural areas with greatest variation in poorest countries. People with diabetes, high blood pressure, or obesity had higher rates of use of the 4 medications.8 Use of proven drugs was consistently lower in current smokers, than in former smokers or never smokers regardless of the economic status of the country, but lowest in smokers in poor country.8
- For people with CAD, there was a significant decline in use of antiplatelet drugs, ACE inhibitors or ARBs, and statins, but not β blockers, with increasing number of years between the index event and time of assessment.8 . Some individuals may feel healthy several years after an acute CVD event or feel that they are at lower risk for an event (e.g., the young), contributing to a decline in their use with time.8 These findings also suggest a need to re-educate both doctors and their patients about the crucial role of medications in secondary prevention.
- For every group of countries, classified by economic development, rates of drug use were consistently lower in rural than urban settings. Once these factors were accounted for, individual-level factors such as age, sex, educational status (a surrogate for economic status), hypertension, diabetes, smoking, and obesity were related to the rates of drug use.8
- Use of proven effective drugs did not differ much between those with CAD alone, stroke alone, compared with those who had stroke and CAD or those who had multiple events. However, use of statins or β blockers was substantially lower when an individual had both events compared with coronary heart disease alone.8
- Surprisingly, some very high risk groups (those with or both CAD and stroke) did not have a higher rate of use of drugs. This finding is consistent with other studies supporting the “inverse care law” (the sickest patients receiving the least care). For instance, 58% of individuals with CAD and 50% of individuals who had a stroke did not receive any of the four effective drug types; these rates were highest in the low-income countries.8 Substantial opportunities remain for enhancement of drug use, even in high-income countries.
|
Table 128A. Potential causes for the underuse of effective medications |
|
| Yusuf S et al. Use of secondary prevention drugs for cardiovascular disease in the community in high-income, middle-income, and low-income countries (the PURE Study): a prospective epidemiological survey. Lancet. Aug 26 2011. |
- The potential reasons for the global underutilization of secondary prevention medications is given in Table 128 A. As the use of secondary prevention medications is low worldwide—especially in low-income countries and rural areas—systematic approaches are needed to improve the long-term use of basic, inexpensive, and effective drugs.8 A major, systematic medical-pharmacological-media campaign should be mounted to reduce the rate of recurrent attacks by using all the recommended medications used in secondary prevention.
Sources
1. American Heart Association. Heart and Stroke Statistical Update2011.
2. Enas EA, Singh V, Munjal YP, Bhandari S, Yadave RD, Manchanda SC. Reducing the burden of coronary artery disease in India: challenges and opportunities. Indian Heart J. Mar-Apr 2008;60(2):161-175.
3. Enas EA, Singh V, Gupta R, Patel R, et al. Recommendations of the Second Indo-US Health Summit for the prevention and control of cardiovascular disease among Asian Indians. Indian Heart J. 2009;61:265-74.
4. Kumar A, Fonarow GC, Eagle KA, et al. Regional and practice variation in adherence to guideline recommendations for secondary and primary prevention among outpatients with atherothrombosis or risk factors in the United States: a report from the REACH Registry. Crit Pathw Cardiol. Sep 2009;8(3):104-111.
5. Sharma KK, Gupta R, Agrawal A, et al. Low use of statins and other coronary secondary prevention therapies in primary and secondary care in India. Vasc Health Risk Manag. 2009;5:1007-1014.