Tertiary Prevention
- Tertiary care hospitals are springing up throughout the world especially India to make full use of Triumphant Procedures in Cardiology that can result in catastrophic health expenditures and distress financing especially those in the lower and middle socio-economic strata.
- Tertiary prevention usually refers to the use of expensive coronary interventional procedures such as coronary angioplasty, stent, bypass surgery, pacemakers, defibrillators, and left ventricular assist devices (LVAD).
- In 2006, an estimated 1.3 million coronary angioplasty/stent procedures, 448,000 bypass procedures, 1.1 million diagnostic cardiac catheterizations, 114,000 implantable defibrillators, and 418,000 pacemaker procedures were performed for inpatients in the US.1 Many of these procedures are also done in outpatients and are not included in these figures.
- People with low incomes from high income countries in North America and Europe are going to low income countries such as India and Thailand for cardiovascular and other procedures that they cannot afford in their home countries. Ironically, the rich, powerful and politically connected are coming to the US precisely for the same procedures.
Coronary Angioplasty/Stent
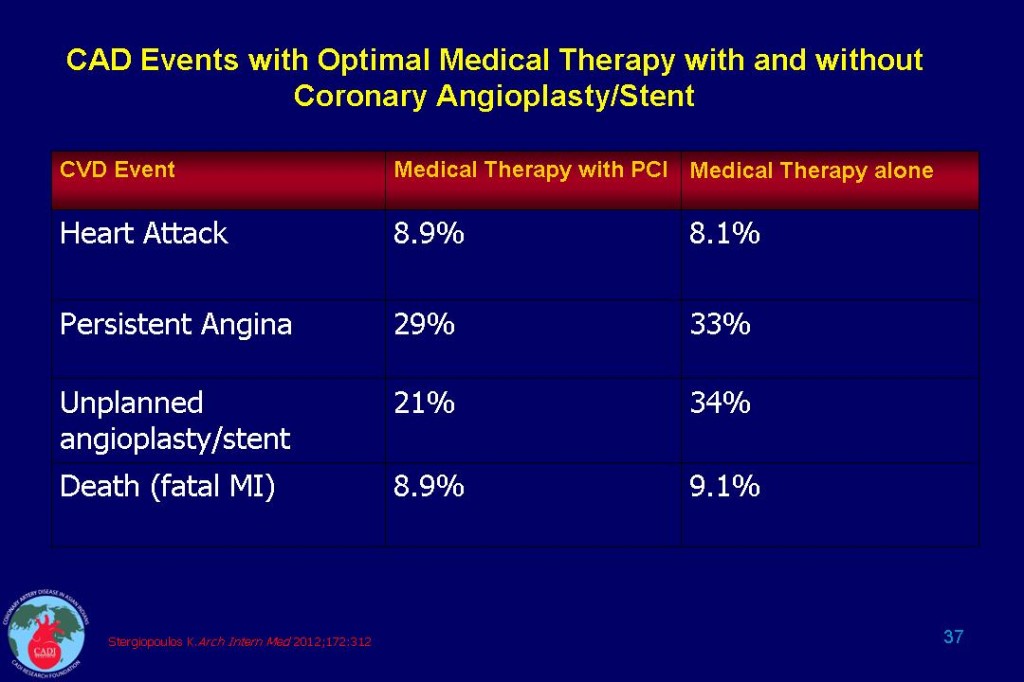
- According to a new meta-analysis, stent placement offered no more benefit than optimal medical therapy in patients with stable coronary artery disease (CAD). In clinical trials conducted in the era of modern medical treatment, stenting plus medical intervention did not significantly reduce the risk of death compared with medical intervention alone. Specifically, stents had no significant effect on the risk of death, heart attack, revascularization, or persistent angina (see Table 37)2. However, stenting can be life-saving in patients having a heart attack.
- The meta-analysis included eight trials with a total of 7,229 patients, including the landmark COURAGE trial. The study contradicts some earlier meta-analyses, which did find improvements in mortality and angina for patients assigned to undergo initial percutaneous coronary intervention (PCI) such as angioplasty or stent. However, those analyses included older studies when medical treatment was not as effective as it is now.2
- Approximately 400,000 PCI procedures are done every year in the US for stable angina. A heart attack from rupture of plaque occurs in 5-30% of patients receiving stent which may be due to placement of the stent itself. Only 44% of the patients are treated with optimal medical therapy prior to PCI.2
- Small, lipid-rich, vulnerable plaques that are angiographically unimpressive and hemodynamically insignificant are responsible for most cases of fatal and nonfatal heart attacks, whereas large, stable plaques that produce angiographically severe stenosis generally result in stable angina but rarely result in heart attack. Accordingly, lipid-optimizing therapy, which stabilizes the vulnerable plaques, may have a major impact on prevention of heart attack and death, whereas revascularization procedures, which are directed at severely stenotic lesions, may not.3 This study has scientifically and convincingly proved this inconvenient truth.
- These results suggest that up to 76% of patients with stable CAD can avoid PCI altogether if treated with optimal medical therapy. Such an approach would result in a lifetime savings of approximately $9,450 per patient in healthcare costs. One study suggested that if one-third of elective PCI procedures in patients with stable disease could be averted or deferred, the associated cost savings would fall between $6 billion and $8 billion annually in the US.4
- The findings support current guidelines, which prefer initial medical treatment with aspirin, statins, angiotensin-converting enzyme inhibitors, or angiotensin receptor blockers, combined with lifestyle changes.
Left Ventricular Assist Device (LVAD)
- A significant number of patients with late-stage heart failure are now considered for heart transplant. However, due to the scarcity of donor hearts, less than 3,000 per year receive it in the US out of a pool of more than 30,000 eligible patients. As a result mechanical pumps, once considered a rare application, have found their place in the mainstream care of end-stage heart failure patients.
- LVADs were developed as a temporary bridge while patients wait on a donor, but the second generation (2005) is so improved that a growing number of patients are having them installed long-term. Mr. Cheney’s LVAD may be cutting edge, but it has the feel of a cell phone from the 1980s. The pumps will become smaller, less invasive, and perhaps one day replace the heart altogether. A defibrillator was once the size of a washing machine.
- The advances in bearing technology, including the replacement of cyclic with continuous flow pumps, the reduction in size and conversion from pneumatic to electric power, have made LVADs a feasible therapy for these patients. The technologic advances have extended pump lifespan from 1-2 years to 4-5 years and allowed patients to return to a full and active life with the device providing a significant portion of the cardiac output to assist the weakened left ventricle.
- Engineering research continues in the areas of smaller pumps; induction-charged batteries that can be implanted to eliminate the skin breach for power wires that often leads to infection; and smaller incisions for implantation. There is even early research on VAD implantation using percutaneous techniques. Medical care is advancing to better understand the bleeding complications related to clotting factor changes, prevention of infections and pump settings to optimize function and minimize complications. Fully computerized pump control will eventually adjust the pump to exercise, rest, sleep and other unique demand situations (as has happened with pacemakers).
- LVADs, once solely implanted in patients awaiting heart transplant (bridge to transplant), have increasingly replaced the need for transplants and are now a long-term option. They have allowed some patients to avoid the complex medication regimens and surgical complications that accompany a heart transplant. These devices may even replace the heart completely in the future, a thought that is fascinating for the future of our profession.
- The economic cost of tertiary prevention is 50-100 times higher than secondary prevention which when applied to the fullest extent may reduce or minimize the need of the vast majority of cardiac procedures.
Sources
1. American Heart Association. Heart and Stroke Statistical Update2011.
2. Stergiopoulos K, Brown DL. Initial Coronary Stent Implantation With Medical Therapy vs Medical Therapy Alone for Stable Coronary Artery Disease: Meta-analysis of Randomized Controlled Trials. Arch Intern Med. Feb 27 2012;172(4):312-319.
3. Enas EA. Testing the efficacy of lipid-lowering therapy versus revascularization: the time has come, or is it past due? Circulation. Jun 30 1998;97(25):2584-2586.
4. Boden WE, O’Rourke RA, Teo KK, et al. Impact of optimal medical therapy with or without percutaneous coronary intervention on long-term cardiovascular end points in patients with stable coronary artery disease (from the COURAGE Trial). Am J Cardiol. Jul 1 2009;104(1):1-4.